Abstract
INTRODUCTION
Prolonged cytopenias following Chimeric Antigen Receptor (CAR) T-cell therapy are common. The cytopenias are mainly due to the genotoxic effects of conditioning chemotherapy and systemic inflammatory insult to hematopoietic stem and progenitor cells from CAR T-cell activity. Tocilizumab, an anti-IL6 receptor antibody, reduces cytokine release syndrome (CRS), a clinical manifestation of CAR T inflammatory toxicity. We sought to determine if prophylactic tocilizumab can decrease the risk and/or severity of CRS. We secondarily hypothesized that decreasing the inflammatory injury to hematopoietic stem cells could improve bone marrow function after CAR T. Lastly, we analyzed the association between cytopenias and CAR T efficacy generally.
METHODS
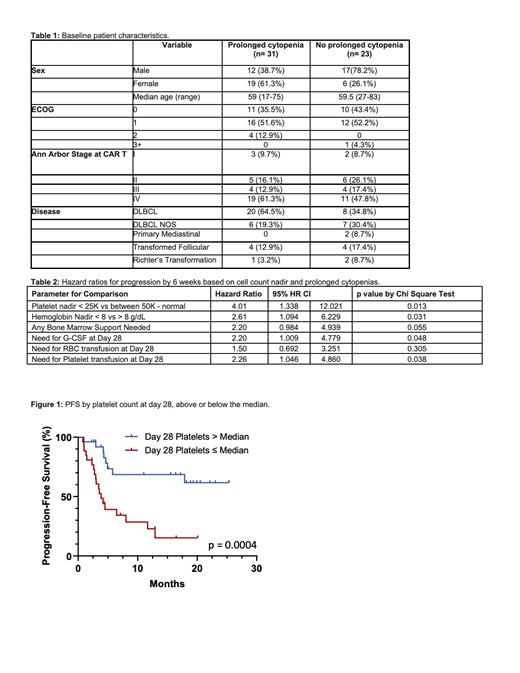
In this single-institution, retrospective cohort study, we examined all patients who had received axicabtagene ciloleucel for relapsed/refractory diffuse large B cell lymphoma (DLBCL) between March 2018 and April 2021 (Table 1). Each patient was evaluated for prolonged cytopenias, defined as requiring granulocyte-colony stimulating factor (G-CSF), red blood cell or platelet transfusion beyond day 28 after CAR T infusion. After CAR T infusion, no patient was given any anti-lymphoma therapy prior to collection of blood count data. We compared response to CAR T 6 weeks post-infusion, progression-free survival (PFS), and overall survival (OS) for patients with and without prolonged cytopenias. A univariate regression analysis was performed, and between group differences were calculated using Chi-squared, Fisher's exact tests, and Cox Proportional hazard regression model. Kaplan-Meier and log-rank analyses were used to evaluate the PFS and OS. We also compared patients who did and did not receive prophylactic tocilizumab 36 hours after CAR T infusion for differences in prolonged cytopenias, PFS, OS, and development and severity of CRS and neurotoxicity. CRS and neurotoxicity were graded using the ASTCT consensus grading system.
RESULTS
The study included 54 patients, 31 (57.4%) met criteria for prolonged cytopenias. 1 (1.9%) patient died of progressive disease prior to day 28 and was excluded from analysis. All patients who died in this study did so on the basis of progressive lymphoma. Likelihood of no response to CAR T at 6 weeks was higher in patients who needed G-CSF support past day 28 (HR 2.20, p = 0.048), had a hemoglobin nadir less than 8 g/dL (HR 2.61, p = 0.031), were still requiring platelet transfusions after day 28 (HR 2.26, p = 0.038), or had a platelet nadir less than 25,000 per µl during the first 28 days (HR 4.01, p = 0.013, Table 2). For patients who had neutrophil counts below the median at day 28, the median PFS was 4.5 months vs. 17.9 months (HR 2.07, p = 0.035) compared to those above the median. In patients with a platelet nadir less than 25,000 per µl or below the median at day 28 (Figure 1), the median PFS was 4.5 months vs. not reached (HR 3.12, p = 0.003) and 3.9 months vs. not reached (HR 3.85, p = 0.0004) respectively. Median OS was 9.44 months in patients who required G-CSF support past day 28 (HR 2.79, p = 0.022) vs. not reached in those who didn't receive G-CSF past day 28. For patients with an ANC below the median on day 28, median OS was 19.87 months vs not reached (HR 2.65, p = 0.022). In patients with a platelet nadir less than 25,000 per µl or below the median at day 28, the median OS were 7.8 months vs not reached (HR 3.72, p = 0.006) and 7.79 months vs not reached (HR 3.39, p = 0.007) respectively. Among patients who received prophylactic tocilizumab, 12 (54.5%) had prolonged bone marrow failure compared to 19 (57.6%) among those who did not (p = 0.82). PFS, OS, and rates and severity of CRS and neurotoxicity did not differ between the prophylactic tocilizumab groups.
CONCLUSIONS
In this study of patients with relapsed/refractory aggressive B-cell lymphomas receiving a CD28 domain-containing CAR T product, severe short-term or prolonged cytopenias were associated with an increased risk of lymphoma progression and death. This effect was not ameliorated by administration of prophylactic tocilizumab, which also did not affect the development or severity of CAR T inflammatory toxicities. Further study is required to determine the mechanistic nature of the relationship between post-infusion cytopenias and CAR T efficacy.
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal